JULY - WOMEN’S HEALTH MONTH
For the month of JULY we will be focusing on women’s Health, particularly Cervical Screening.
Cervical cancer is one of the most preventable cancers. Regular cervical screening and human papillomavirus (HPV) immunisation are the best ways to protect yourself.
Screening allows for early detection, follow-up testing and treatment. It finds early warning signs before they become cancer. Of the 180 people who get cervical cancer in Aotearoa New Zealand every year, 85% have either never been screened or have not had regular screening.
Sneak peek at what we have in store for July…
CERVICAL SCREENING CLINICS FOR JULY
Lunchtime Drop-In Clinics
Have some spare time over lunch? Pop into our drop-in clinics Monday to Friday between 12 & 2 for the month of July. No appointment needed. One of our nurses will be free to see you and run through any questions you may have.
THURSDAY EVENING Clinics
On the 4th, 11th, 18th & 25th July we will be running evening clinics for those who work during the day and cannot attend our lunch time drop-in clinic. These sessions will be between 5 & 6pm on a Thursday. Please contact us to make a booking on 03 578 0199
unable to attend either and due or overdue your cervical screening?
Request a call back by completing the form below if you have any queries. One of our nurses will be in touch.
DOING AN HPV SWAB (SELF-TEST)
The vaginal swab is an easy way for most people to collect their screening sample. It is quick and should not be uncomfortable.
You will usually do a self-test at your screening appointment after your consultation. You can do the test in private behind a screen or in a bathroom. You may be able to take your test home and bring it back when you are done, talk to our team if you are interested in this.
If you make a mistake
It is very unlikely you will get anything wrong.
It is okay to continue with the test if you:
have touched the swab tip with your fingers (though it is best to avoid this)
have inserted the swab into your vagina but are unsure if you have inserted it far enough.
If you drop your swab let your healthcare provider know and ask them for a replacement.
-
If you choose to do a self-test you will be given a kit with detailed instructions.
If you have any questions or difficulty, ask your healthcare provider for help.
Step 1
Wash your hands with soap and water and dry them thoroughly.
Step 2
In a private space, find a comfortable position to take your sample. You may like to sit, stand, lie down or squat. If you cannot find a position that works for you, ask your healthcare provider for help.
Step 3
Take the tube containing the swab out of the bag and remove the swab stick. You may need to hold and twist the cap to break the paper seal.
Try not to touch the swab tip either with your fingers or against any surface.
Step 4
Holding the swab stick halfway down, use your free hand to open your vagina and gently insert the tip of the swab about 4 to 5cm (about the length of your thumb, similar to inserting a tampon).
Most people find it easy and comfortable to do. If you experience any pain, then draw the stick back a bit until it is more comfortable or ask your healthcare provider to assist.
Step 5
Rotate the swab 4 times for about 20 seconds, gently touching the sides of the vagina, then remove. Put the swab back into the tube.
Step 6
Once you have collected your sample, check the kit instructions for next steps on what to do with the swab. Make sure the cap on your sample is put on tightly, so it is well-sealed.
Step 7
Dispose of any leftover materials in the rubbish bin, then wash your hands with soap and water and dry them thoroughly.
Step 8
Place the completed sample and form back into the bag, seal it and give it back to your healthcare provider who will send it for testing.
Note: The self-test is not like a RAT or pregnancy test — it will not show you results. Your swab will be sent to a lab for testing to get your results.
How to do a vaginal swab (self-test) — Rainbow community
How to do a vaginal swab (self-test) - English
How to do a vaginal swab (self-test) — Te reo Māori
How to do a vaginal swab (self-test) — Pacific
How to do a vaginal swab (self-test) — New Zealand Sign Language
LOOK OUT FOR OUR MAILBOXES TO DROP YOUR SWAB!
We have 2 dedicated mailboxes for patients to drop their self-swabs into.
One located at the front entrance of the practice and
One located in our patient toilet.
Both options are discreet and no need to hand your swab to reception. Pop it in the mailbox and our team will collect the samples during the day and be in touch once your results are back.
WHAT’S THE COST FOR AN HPV SELF-SWAB?
Here at CIVIC we offer FREE Cervical Screening to all women and those with a cervix who are enrolled with the practice. Contact us today if you have any queries or have not had any screening done before or are overdue due to financial barriers.
ADDITIONAL INFORMATION AND RESOURCES
Information and page credit to Cervical screening | Time to Screen - National Screening Unit
ABOUT HPV AND CERVICAL CANCER
-
About Human PapillomaVirus (HPV)
About 4 out of 5 adults will have HPV at some time in their lives. It is spread through intimate skin-to-skin contact and any sexual activity. While HPV often clears up by itself, it can stay dormant in your system and may not be detected until years after you come into contact with it. If found in a test, this may not be due to a new exposure with HPV. This is why regular, ongoing screening is still important even if you have been with the same partner, or not been sexually active for sometime.
People with HPV usually:
do not have symptoms
do not know they have it
have no problems or complications.
There are many different types of HPV, and some are more likely than others to lead to cervical cancer.
The body is pretty good at clearing the virus itself, usually within 2 years, especially in people under 30. However, sometimes it can persist and may develop into cervical cancer over time. 95% of cervical cancers are caused by HPV.
Having HPV does not mean you have cancer.
-
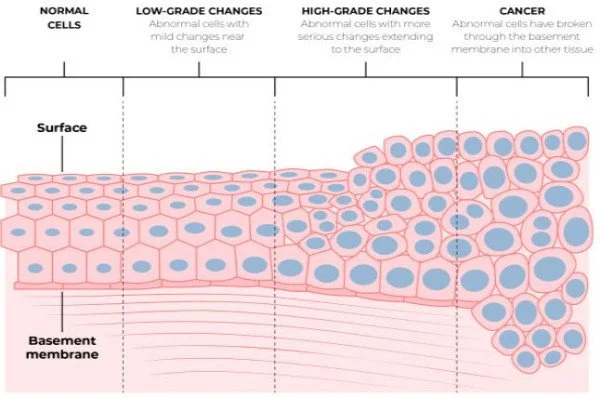
Cervical cancer starts in the cells lining the cervix. This is triggered by cell changes usually caused by the human papillomavirus (HPV).
Cervical cancer can take 10 years or more to develop.
The cell changes caused by HPV may return to normal by themselves. In a small number of cases they develop into cancer if left untreated.
It is impossible to tell which abnormal cells will return to normal, and which may go on to become cancer. That is why regular screening tests are so important.
Types of cervical cancer
The 2 main types of cervical cancer are:
squamous cell cancer — forms in the cells where the vagina meets the cervix
glandular cell cancer — forms in the glandular cells that line the cervical canal.
Squamous cell cancer is found in about 80% of people with cervical cancer, and glandular in 15%.
Cervical cancer symptoms
Cell changes themselves do not usually cause any symptoms, and some symptoms may only appear once they become cancer. Regular cervical screening helps to find these changes early, so treatment can be provided before cancer develops.
Visit your doctor or nurse if you notice anything unusual, like:
bleeding or spotting between periods or after your periods have stopped (after menopause)
pain during sex
bleeding or spotting after sex
vaginal discharge that is not normal for you
persistent pain in your pelvis or lower back.
These symptoms can happen for many reasons. They rarely mean you have cervical cancer. However, it is still important to get them checked out by a health professional.
Risk factors for cervical cancer
Risk factors for developing cervical cancer include:
having HPV that does not clear up
smoking
not being immunised against HPV.
-
With HPV immunisation and HPV testing, Aotearoa New Zealand aims to eliminate cervical cancer in the future.
Preventing cervical cancer
Cervical cancer often takes 10 or more years to develop. With regular screening, abnormal cells can be found and treated early before they become cancer.
The HPV screening test is able to pick up cell changes very early. Most people will only need to have an HPV screening test every 5 years.
The HPV vaccine
Regular cervical screening, along with immunisation against HPV, is the best protection against cervical cancer.
Find out about the vaccine, who needs it and when to get it on the Te Whatu Ora Immunise website.
-
There are 4 other types of gynaecological cancers that are currently not screened for:
ovarian
uterine
vulval
vaginal.
You can learn more about other types of cancers on:
-
Cell changes on the cervix happen very slowly. There are many stages between HPV infection, cell changes and cancer.
CERVICAL screeNING OPTIONS
-
In September 2023, HPV screening became the new method for cervical screening in Aotearoa New Zealand. HPV testing is a better first screening test. It looks for the human papillomavirus (HPV), which causes cell changes that may lead to cervical cancer.
This gives you options for how you have your screening sample taken:
a vaginal swab — you can either self-test, or a health professional can help
a cervical sample (previously known as a smear test) — taken by a health professional.
-
Your healthcare provider can help you find out which type of test is better for you.
The vaginal swab is quick and easy to do. But this may not be suitable for everyone. Some people may be recommended to have a cervical cell sample taken (previously known as a smear test) depending on their screening history.
Some people may also prefer to have their sample taken as a cervical sample. A cervical sample also tests for HPV.
If you do a vaginal swab test and HPV is found, you will either be recommended to return to have a cervical sample taken as a follow-up test, or referred directly to colposcopy. This will depend on the type of HPV detected.
-
If you have your period
If you have your period, you can still have a screening test as long as the bleeding is not too heavy. This could affect the test result.
During pregnancy
It is safe to have a screening test when you are pregnant, but it is best to discuss this with your healthcare provider.
After pregnancy
After the birth of your baby, you should wait 6 weeks to have your screening test. This allows time for the changes from pregnancy to settle.
If you need extra support
You may take a support person with you to your appointment. When booking, let your healthcare provider know if you:
have a disability that means you need extra support
need an interpreter.
-
Your HPV result will usually come back within 1 to 2 weeks. Talk to your healthcare provider about how you want to be contacted.
Most test results are normal — around 90% do not find HPV.
However, it is important to continue to have regular screening.
If HPV is found, depending on which test you have and the type of HPV found, you may be recommended to have a cervical cell sample taken or you may be referred for colposcopy for treatment if needed.
Find more information about the next steps.
-
The National Cervical Screening Programme is not fully funded. However, free screening is available for women and people with a cervix who:
are Māori or Pacific, any age
are 30 years and over who are under-screened (have not had a test in the past 5 years), or have never had a screening test
require follow-up testing, any age
hold a Community Services Card, any age.
For more information about what screening tests are funded, and what follow-up tests are funded, download our guide.